Spinal Neurofibromas in NF1
The following is a blog by Dr. Luiz Rodrigues . Originally posted in Portuguese on July 3 2017. Additions and translation were provided by Dr. Mata-Machado from the NF Clinic at Amita Health/St. Alexis.
“The doctor said my daughter has more internal neurofibromas near the spinal cord than external ones on the skin. What does that mean? ” – BAH, from Portugal.
Cara B, thank you for your question, but to guide your family, I need to see your daughter in person or get a report from her doctor. Anyway, I will answer in general terms on this subject, which is spinal neurofibromas in people with NF1.
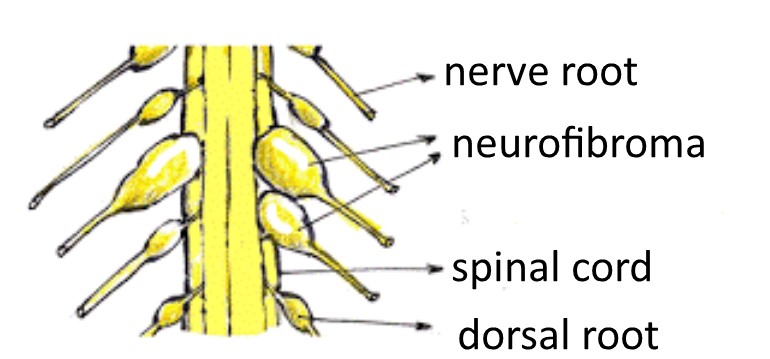
There are different types of neurofibromas including cutaneous, diffuse subcutaneous, nodular subcutaneous and plexiform (see HERE for descriptions of each). Spinal neurofibromas are usually of the nodular subcutaneous type, although commonly plexiform neurofibromas start in a nerve root and spread to other parts of the body.
About 30% of people with the most common forms of NF1 (which are point mutations within the gene) have one or more neurofibromas in the roots of nerves coming out of the spinal cord. This percentage of spinal neurofibromas increases to 64% in people with complete deletion of the NF1 gene (learn more about gene deletion HERE).
Throughout life, these neurofibromas usually go without causing problems or symptoms. In some people they may increase in size and compress the spinal cord and other nerves and structures in that region, interrupting the nervous communication between the brain and any part of the body. This compression can lead to pain, or loss of muscle strength or sensitivity.
In some people with NF1, neurofibromas in the roots of the spinal nerves can also damage the vertebral bodies, causing neurological complications (loss of strength and movement) and orthopedic complications (scoliosis) especially in the neck and sacral loins.
Spinal form of NF1
There is also a rarer form of NF1 (1 to 60 thousand people) in which the formation of spinal neurofibromas occurs in all nerve roots on both sides of the body. This is special phenotype we call the “spinal form” of NF1. This form usually appears in more than one member of the same family (when NF1 is hereditary). In addition, this spinal form affects the major peripheral nerves (such as the sciatic) and has a greater tendency for malignant transformation of one or more of these neurofibromas.
A review of 2015 (see HERE) studied a group of 98 people with the supposed spinal form of NF1, aged between 4 and 74 years. Most of them (49) had neurofibromas in all nerve roots, but the other 49 had multiple spinal neurofibromas, but not at all roots. In addition, the most involved genetic mutations in the spinal form were missense coding errors of the gene.
It is important to note that in the spinal form the other manifestations of NF1 (such as multiple cutaneous and plexiform neurofibromas) are usually absent and café au lait spots may be less than 5 and there may be no ephelides (freckling). The definite diagnosis of the spinal form of NF1 requires full body resonance.
The spinal form can produce symptoms at any time of life, from infancy and especially in adolescence, up to 50 years of age. I recently attended to a 54-year-old at the Neurofibromatosis Reference Center Neurofibromatoses in the Hospital das Clínicas who, despite having shown some reduction in leg strength since the age of 18, only in the last six years has become incapable of working. It was increased spinal cord compression that forced him to become a wheelchair. More information on the spinal form can be obtained
HERE.
Surgical treatment of spinal neurofibromas should only be considered when they produce significant symptoms because of compression, such as severe pain, loss of neurological function or suspicion of malignancy. However, it is a time-consuming, complex surgery that has its own risks, such as hemorrhage, infection of the nervous system, and instability of the spine in the postoperative period. For this reason, most neurosurgeons are hesitant to perform surgery, especially on the spine (reaching all nerve roots), where determining the exact origin of the symptoms is practically impossible. In addition, one study showed a higher incidence of postoperative complications in people with NF1 than in others treated for the removal of spinal tumors (see HERE). Unfortunately, the medical literature on the treatment of these spinal neurofibromas is small. One of the reviews on the subject that I had access to (kindly shared with me by Dr. Vincent M Riccardi) is from 1998 (see HERE). In this review, the majority of surgically treated cases presented improvement in neurological function. Therefore, when it is possible to locate the neurofibroma in the nerve root that is causing the pain or the loss of function, surgery for the decompression may be helpful by the partial or complete removal of the neurofibroma.
Some people with NF1 and spinal neurofibromas in the cervical region have been operated on at our Hospital das Clínicas with encouraging results so far. There were three people with NF1 who arrived at our Reference Center in wheelchairs or with severe loss of muscle strength in their legs and arms, “disillusioned” by surgeons in their hometowns, who are walking today and leading a better life after surgery performed by neurosurgeon Eric Grossi Morato and his team. Their surgical technique, especially aimed at these neurofibromas in people with NF1, consists of reducing the size of tumors (without intending to remove them completely) and make room for the tumors to not compress the marrow if they grow again in the future. In addition, Dr. Eric does not open the dura (the membrane that lines the spinal cord) which prevents the loss of cerebrospinal fluid, as well as infections and fistulas. In summary, the existence of spinal neurofibromas is one of the consequences of neurofibromatosis type 1, which may or may not cause complications. I know people with NF1 who have neurofibromas on the spine for decades with very few or no significant symptoms leading a normal life. Others presented symptoms of spinal cord compression in adolescence that required surgical intervention. Still, others have presented symptoms of compression without possibility of surgical treatment, but control their symptoms with medicines. As we know, this demonstrates the great variability of NF1 manifestations between one person and another. Each person has a different story. In summary, people with spinal neurofibromas need regular and detailed medical reevaluations with a neurofibromatosis specialist.







.png)





